Article Plan: Implant Post Op Instructions PDF
This comprehensive PDF guide details crucial post-operative care following dental implant surgery, ensuring optimal healing and long-term implant success for patients․
Dental implant surgery is a transformative procedure offering a permanent solution for missing teeth, restoring both function and aesthetics․ Unlike traditional options, implants fuse with the jawbone – a process called osseointegration – providing a stable and natural-feeling replacement․ This guide focuses on the critical post-operative period, outlining essential instructions to ensure successful healing and minimize complications․

Proper care following implant placement is paramount․ Understanding these guidelines, from pain management to dietary restrictions, will significantly contribute to a smooth recovery and the longevity of your new smile․ This PDF serves as your resource for navigating the initial stages of healing․
Understanding the Immediate Post-Operative Period (First 24-48 Hours)
The initial 24-48 hours following dental implant surgery are crucial for initiating the healing process․ Expect some discomfort, swelling, and potentially bruising – these are normal responses to the procedure․ Rest is paramount; avoid strenuous activity and prioritize relaxation․ Gentle bleeding is also common, manageable with gauze provided by your surgeon․
Focus on adhering to prescribed medication schedules for pain and potential infection prevention․ Maintaining a soft diet and diligent oral hygiene, as outlined in this PDF, will further support optimal healing during this sensitive period․ Contact your surgeon with any concerns․
Pain Management After Implant Placement
Effective pain management is vital for a comfortable recovery after dental implant surgery․ While some discomfort is expected, it should be manageable with a combination of strategies․ This PDF guide outlines options ranging from over-the-counter analgesics to prescription pain medication, as directed by your surgeon․
Proactive pain control, starting immediately post-op, is recommended․ Don’t wait for the pain to become severe before taking medication․ Remember to follow dosage instructions carefully and report any adverse reactions․ Combining medication with ice packs and rest enhances pain relief․

Over-the-Counter Pain Relief Options
For mild to moderate post-operative pain, over-the-counter (OTC) pain relievers can be highly effective․ Ibuprofen (Advil, Motrin) and naproxen (Aleve) are nonsteroidal anti-inflammatory drugs (NSAIDs) that reduce both pain and swelling․ Acetaminophen (Tylenol) is another option, primarily targeting pain relief․
This PDF guide recommends alternating between ibuprofen and acetaminophen, following package directions, to maximize comfort․ Always inform your surgeon of any existing medical conditions or medications before taking OTC pain relievers, to avoid potential interactions․
Prescription Pain Medication Guidelines

If over-the-counter medications are insufficient, your surgeon may prescribe stronger pain relief․ This PDF details crucial guidelines for prescription use: take medication exactly as prescribed, do not exceed the recommended dosage, and avoid combining it with alcohol or other sedatives․
Be aware of potential side effects, such as drowsiness or constipation, and contact your surgeon if they become bothersome․ Properly dispose of any unused medication to prevent accidental ingestion․ Never share your prescription with others;
Controlling Swelling and Bruising
Post-implant surgery swelling and bruising are normal, peaking around 48-72 hours․ This PDF outlines strategies for minimizing these effects․ Immediately following the procedure, apply ice packs to the outside of your face in 20-minute intervals, ensuring a cloth barrier protects your skin․
Elevate your head with extra pillows, even while sleeping, to reduce blood flow to the surgical area․ Avoid strenuous activity, as it can exacerbate swelling․ These measures will significantly contribute to a more comfortable recovery․
Ice Pack Application Protocol
This PDF details the proper ice pack application for optimal swelling control after implant surgery․ Begin immediately post-op, applying an ice pack to the outside of your cheek in the treated area․ Use a cloth barrier between the ice and skin to prevent discomfort․
Apply for 20 minutes on, then remove for 20 minutes off․ Continue this cycle for the first 48-72 hours․ Consistent application, following this protocol, significantly reduces swelling and discomfort, promoting faster healing and a more comfortable recovery process․
Head Elevation Recommendations
This PDF emphasizes the importance of head elevation post-implant surgery to minimize swelling and discomfort․ For the first 48-72 hours, sleep with your head elevated on 2-3 pillows․
Even when resting during the day, maintain this elevated position․ This helps to reduce blood flow to the surgical site, effectively controlling swelling and bruising․ Avoid bending over or strenuous activity that could increase pressure in the head and neck region, further aiding the healing process and ensuring optimal results․

Wound Care and Hygiene
This PDF details essential wound care following implant placement․ Avoid disturbing the surgical site with your tongue or fingers․ Gentle cleaning is paramount; after 24 hours, begin rinsing with warm salt water (1/2 teaspoon salt in 8oz water) after each meal․
Do not vigorously rinse or spit․ This PDF also outlines proper chlorhexidine mouthwash usage, as prescribed by your surgeon, to maintain a sterile environment and prevent infection, promoting optimal healing and implant integration․
Gentle Cleaning Instructions
This PDF emphasizes gentle oral hygiene post-implant surgery․ Begin with soft-bristled toothbrushing around the implant site, avoiding direct pressure on the surgical area․ Use a gentle, circular motion․ Avoid toothpaste for the first few days, transitioning to a mild, non-abrasive formula as healing progresses․

Carefully floss around adjacent teeth, being cautious not to disrupt the surgical site․ This PDF stresses the importance of consistent, yet delicate, cleaning to prevent plaque buildup and promote optimal tissue healing around the new implant․
Chlorhexidine Mouthwash Usage
This PDF details proper chlorhexidine mouthwash application post-implant placement․ Rinse gently for 30-60 seconds twice daily, typically starting 24 hours after surgery, as directed by your surgeon․ Do not swallow the mouthwash․ It aids in reducing bacterial load and preventing infection․
Be aware that chlorhexidine can cause temporary tooth staining; this is harmless and will be addressed during your routine cleaning․ This PDF advises against prolonged use, as it can disrupt oral flora․ Follow your surgeon’s specific instructions regarding duration․

Dietary Restrictions – What to Eat and Avoid
This PDF outlines essential dietary guidelines post-implant surgery․ Initially, a soft food diet is crucial – think yogurt, applesauce, mashed potatoes, and smoothies․ Avoid hard, crunchy, chewy, or spicy foods that could irritate the surgical site or damage the implant․
Steer clear of small seeds, nuts, and anything requiring significant chewing effort․ Gradually reintroduce firmer foods as healing progresses, guided by your surgeon’s advice․ Maintaining adequate nutrition supports optimal healing and osseointegration․
Soft Food Diet – First Week
This PDF details the first week’s dietary focus: a strictly soft food regimen․ Excellent choices include yogurt, pudding, applesauce, mashed potatoes, scrambled eggs, and well-cooked cereals․ Broths and clear soups provide hydration and nutrients․ Smoothies are beneficial, ensuring they lack seeds or small pieces․
Avoid any food requiring chewing, like steak or raw vegetables․ Prioritize easily digestible options to minimize strain on the surgical site and promote comfortable healing․ Proper nutrition is vital during this initial phase․
Gradual Return to Normal Diet
This PDF outlines a phased approach to resuming your regular diet․ Starting around week two, slowly introduce softer, easily chewed foods like pasta, fish, and tender chicken․ Monitor for any discomfort or sensitivity at the implant site․ Avoid hard, crunchy, or sticky foods initially, as these can potentially disrupt healing․
Progress gradually, adding more texture as tolerated․ Continue prioritizing nutritious meals to support tissue regeneration․ Listen to your body and adjust your diet accordingly, consulting your surgeon if needed․
Activity Restrictions
This PDF details necessary activity limitations post-implant surgery․ For the first 48-72 hours, prioritize rest and avoid strenuous physical exertion․ Refrain from heavy lifting, vigorous exercise, and activities that could increase blood pressure․ Light walking is encouraged to promote circulation, but avoid overexertion․
Gradually increase activity levels as tolerated, listening to your body’s signals․ Avoid any activity that causes discomfort at the surgical site․ Prolonged bending over or straining should also be minimized during the initial healing phase․
Avoiding Strenuous Exercise
This PDF emphasizes avoiding strenuous exercise for at least one week post-implant surgery, and potentially longer depending on individual healing․ High-impact activities, running, and weightlifting can create pressure and disrupt the osseointegration process․ Increased blood flow from exertion may also lead to swelling and discomfort․
Focus on gentle movements and light walking․ Consult your surgeon before resuming your regular exercise routine․ Prematurely returning to intense physical activity risks complications and can jeopardize the implant’s stability․ Prioritize healing for optimal long-term success․
Limitations on Physical Activity
This PDF details specific physical activity limitations post-implant surgery․ Avoid activities that could potentially impact the surgical site, including heavy lifting (over 10-15 pounds), bending over extensively, and strenuous cardiovascular exercise․ Refrain from activities requiring significant jaw movement or pressure․
These restrictions are crucial for proper osseointegration and preventing complications․ Listen to your body and avoid any activity that causes pain or discomfort․ Gradual resumption of normal activities, guided by your surgeon’s advice, is essential for a successful recovery․
Recognizing and Addressing Complications
This PDF outlines potential post-implant complications․ Be vigilant for signs of infection, including fever (over 100․4°F), increased pain, swelling, redness, or pus discharge from the surgical site․ Excessive bleeding, numbness, or tingling are also concerning․
Promptly address any unusual symptoms․ While some discomfort is normal, escalating pain warrants immediate attention․ Do not attempt self-treatment; contact your surgeon immediately if you suspect a complication․ Early intervention is key to preventing minor issues from becoming serious problems․
Signs of Infection (Fever, Increased Pain, Pus)
This PDF details critical infection indicators post-implant․ A fever exceeding 100․4°F is a significant warning sign․ Noticeable increases in pain, despite prescribed medication, demand attention․ The presence of pus – a thick, yellowish or greenish discharge – around the implant site is a clear indication of infection․
Redness, warmth, and escalating swelling are also concerning․ Don’t ignore these symptoms; they suggest your body is fighting an infection․ Immediate contact with your surgeon is crucial to prevent complications and ensure proper treatment․
When to Contact Your Surgeon Immediately
This PDF emphasizes prompt communication․ Contact your surgeon immediately if you experience uncontrolled bleeding, lasting longer than a few hours with gentle pressure․ A high fever (over 100․4°F) or chills necessitate urgent attention․ Severe, escalating pain unresponsive to medication requires immediate evaluation․
Signs of infection – pus, increasing redness, or swelling – are critical reasons to call․ Difficulty breathing or swallowing also demands immediate medical intervention․ Don’t hesitate; early intervention prevents complications and safeguards your implant’s success․
Sutures and Follow-Up Appointments
This PDF details suture types – often dissolving, sometimes requiring removal․ Keep the area clean to prevent infection around sutures․ Attend all scheduled follow-up appointments; these are vital for monitoring healing and osseointegration․ Your surgeon will assess bone integration and overall implant stability․
Follow-ups allow for early detection of potential issues․ Don’t miss these crucial checks! They ensure long-term implant success and address any concerns promptly․ Consistent monitoring is key to a healthy, functional dental implant․
Types of Sutures Used
This PDF explains that dental implant surgery utilizes various suture types․ Commonly, dissolving sutures (absorbable) are employed, eliminating the need for removal․ However, non-absorbable sutures may be used in certain cases, requiring a follow-up appointment for their removal, typically within 7-14 days․

Suture material selection depends on the surgical site and individual healing needs․ Proper suture care, as detailed in this guide, is crucial to prevent infection and promote optimal wound closure․ Contact your surgeon with any concerns regarding your sutures․
Importance of Scheduled Follow-Ups
This PDF emphasizes that consistent follow-up appointments are vital for successful implant integration and long-term health․ These visits allow your surgeon to monitor healing, assess osseointegration, and address any potential complications promptly; Ignoring scheduled appointments can jeopardize the entire process․
Follow-ups typically occur at intervals of 1 week, 3 months, 6 months, and annually thereafter․ During these visits, radiographs may be taken to evaluate bone levels․ Adhering to the recommended schedule ensures optimal implant function and longevity, preventing future issues․
Long-Term Implant Maintenance
This PDF highlights that dental implants, while durable, require diligent long-term maintenance mirroring natural tooth care․ Consistent oral hygiene – brushing twice daily and flossing – is paramount to prevent peri-implantitis, an inflammation around the implant․
Regular professional cleanings (every 6 months) are crucial for removing plaque and tartar buildup․ Avoid abrasive toothpastes and aggressive brushing, which can damage the implant surface․ Lifestyle factors like smoking significantly impact implant longevity; cessation is strongly advised․ Proactive care ensures a lifetime of functional and aesthetic benefits․
Potential Risks and Complications of Dental Implants
This PDF outlines potential, though uncommon, risks associated with dental implant surgery․ These include infection at the implant site, nerve damage potentially causing numbness or tingling, and sinus problems if implants are placed in the upper jaw․
Implant failure, though rare, can occur due to insufficient bone density or peri-implantitis․ Allergic reactions to implant materials are also possible․ Careful patient selection, meticulous surgical technique, and diligent post-operative care minimize these risks․ Promptly reporting any unusual symptoms to your surgeon is vital;
The Role of Bone Grafting in Implant Success
This PDF details how sufficient bone density is crucial for successful implant osseointegration․ If adequate bone volume is lacking, bone grafting becomes necessary․ Grafting utilizes bone from another site in your body or a donor source to build up the jawbone․
Different grafting techniques exist, including block grafts and sinus lifts․ Post-operative care after grafting is vital for proper healing and integration․ Bone grafting increases implant stability and long-term success rates, ensuring a solid foundation for your restoration․
Osseointegration Process Explained
This PDF clarifies that osseointegration is the cornerstone of implant stability․ It’s the biological process where the implant fuses directly with the jawbone․ This fusion creates a strong, lasting bond, essential for successful function․
The process takes several months, requiring patience and adherence to post-operative instructions․ Factors like bone quality, implant surface, and surgical precision influence osseointegration․ Avoiding excessive force during this phase is critical․ Successful osseointegration ensures a predictable and durable dental restoration․
Smoking and Implant Failure
This PDF emphatically states that smoking significantly increases the risk of dental implant failure․ Nicotine impairs blood flow to the gums, hindering the crucial osseointegration process․ Reduced blood supply compromises bone healing and increases susceptibility to infection․
Patients who smoke experience higher rates of implant loss compared to non-smokers․ Quitting smoking before and after surgery dramatically improves implant success․ This guide strongly advises cessation, offering resources for support․ Continued smoking jeopardizes the investment in your dental health․
Importance of Oral Hygiene for Implant Longevity
This PDF stresses that meticulous oral hygiene is paramount for long-term implant success․ Just like natural teeth, implants require diligent cleaning to prevent peri-implantitis – an inflammation around the implant that can lead to bone loss and eventual failure․
Daily brushing and flossing are essential, alongside regular professional cleanings․ Specialized interdental brushes and floss are recommended․ This guide details proper techniques to effectively remove plaque and bacteria, safeguarding your investment and ensuring a healthy, lasting smile․
Common Post-Operative Symptoms and Their Management
This PDF outlines expected post-operative symptoms, including swelling, bruising, and mild discomfort․ Pain management strategies, like over-the-counter analgesics and prescribed medication (when necessary), are detailed․ It explains how to apply ice packs effectively to minimize swelling and recommends head elevation․
The guide also addresses potential minor bleeding and how to manage it․ Importantly, it clarifies which symptoms are normal and when to contact the surgeon immediately, emphasizing proactive symptom management for a smoother recovery․
Creating a PDF Guide for Post-Op Instructions
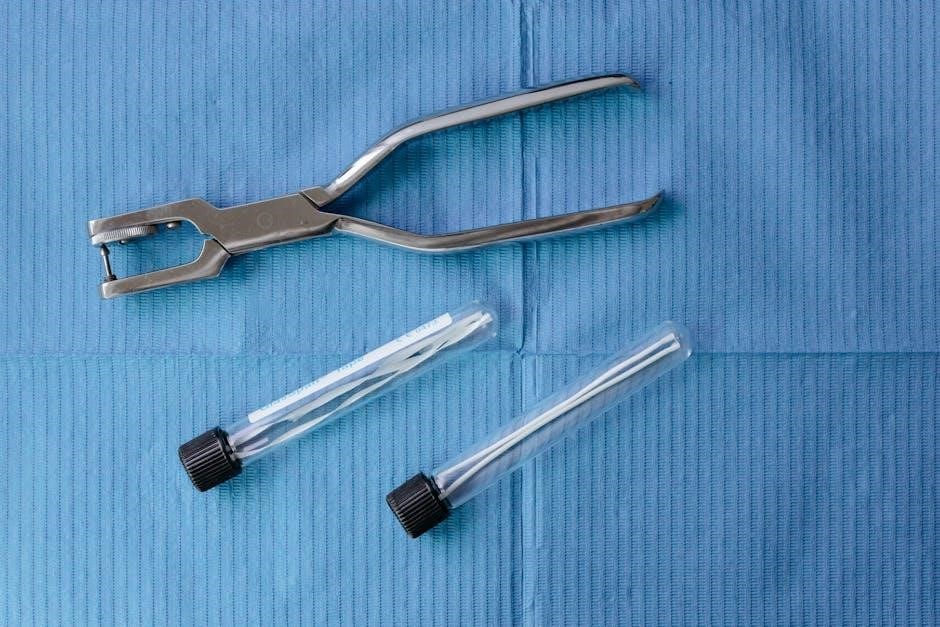
This PDF should be designed for easy readability, utilizing clear headings, concise language, and bullet points for quick reference; Include high-quality images illustrating proper wound care, ice pack application, and dietary guidelines․ Ensure the document is accessible on various devices – computers, tablets, and smartphones․
Prioritize a logical flow, mirroring the patient’s recovery timeline․ A downloadable and printable format is essential․ Consider incorporating a checklist for patients to track their progress and medication schedule, promoting adherence to post-operative care․

Resources for Additional Information and Support
Patients can find supplementary information through the American Academy of Periodontology (AAP) website, offering detailed insights into dental implants and post-operative care․ Numerous online forums and support groups connect individuals undergoing similar procedures, fostering a sense of community and shared experience․
Your dental practice should provide a dedicated contact number for urgent concerns․ Reputable dental implant manufacturers often offer patient education materials․ Encourage patients to utilize these resources to enhance their understanding and actively participate in their recovery journey․
This PDF provides general post-operative guidelines and should not substitute personalized advice from your oral surgeon․ Individual healing experiences vary, and adherence to your surgeon’s specific instructions is paramount․ We are not liable for complications arising from deviations from prescribed care․
For emergencies or concerns outside regular office hours, please contact [Surgeon’s Name] at [Phone Number] or proceed to the nearest emergency room․ Our office address is [Address], and our general inquiries line is [Phone Number]․



